|
 
 |
| ORIGINAL ARTICLE |
|
| Year : 2014 | Volume
: 9
| Issue : 2 | Page : 74-78 |
|
Cardiopulmonary efficiency in gutkha chewers: An Indian study
A Pakkala1, CP Ganashree2, T Raghavendra3
1 Department of Physiology, PES Institute of Medical Sciences and Research, Kuppam, Chittoor, Andhra Pradesh, India
2 Department of Physiology, Basaveshwara Medical College, Chitradurga, Karnataka, India
3 Department of Anesthesiology, Basaveshwara Medical College, Chitradurga, Karnataka, India
| Date of Web Publication | 19-Aug-2014 |
Correspondence Address:
A Pakkala
Department of Physiology, PES Institute of Medical Sciences and Research, Kuppam, Chittoor, Andhra Pradesh
India
 Source of Support: None, Conflict of Interest: None  | Check |
DOI: 10.4103/9783-1230.139168

Background: Smokeless tobacco has been used in various forms orally alone or in combination with other ingredients. In India, tobacco is taken in gutkha form by a large section of the population. Use of gutkha indeed represents a health concern of growing magnitude among these groups. As a consequence of its addictive qualities, the consumption of smokeless tobacco often becomes a lifelong habit with cumulative and deleterious effects on health. Chewable tobacco has been advocated as a substitute for cigarette smoking. On the contrary, the use of smokeless tobacco is fraught with health risk and needs to be discouraged. Previous reports have described long term harmful effects of nicotine on various body parameters, little is known about acute effect of smokeless tobacco on cardiopulmonary parameters. Very few studies have been undertaken on the acute effect of use of gutkha, a common form of smokeless tobacco in India on cardiopulmonary parameters of youngsters. Materials and Methods: Treadmill exercise testing and pulmonary function tests were done before and after maximal exercise testing to assess cardiopulmonary efficiency in two groups' viz., healthy sedentary controls and healthy gutkha chewers. Results: On studying the differences in cardiopulmonary efficiency in the two groups the resting heart rate (HR) was found to be statistically significantly higher in the study group and the delta HR was found to be statistically significantly lower among gutkha chewers. There was no significant difference seen in parameters like maximal oxygen consumption, maximum oxygen pulse, maximum voluntary ventilation, and maximum minute ventilation as an acute effect of gutkha chewing. Conclusion: In this study, it appears that gutkha chewers are physically fit like controls, but after immediate tobacco chewing a lesser delta HR suggests a higher risk for cardiovascular mortality. Stopping gutkha chewing at this juncture can be helpful in reverting back the risk and parameters like resting HR, recovery HR, and delta HR can be used as prognostic assessment tools for any intervention therapy to stop gutkha chewing in asymptomatic individuals. Keywords: Cardiopulmonary, Delta heart rate, Gutkha, Maximum minute ventilation, Maximal oxygen consumption, Maximum voluntary ventilation, Resting heart rate, Smokeless tobacco
How to cite this article:
Pakkala A, Ganashree C P, Raghavendra T. Cardiopulmonary efficiency in gutkha chewers: An Indian study. J Med Investig Pract 2014;9:74-8 |
How to cite this URL:
Pakkala A, Ganashree C P, Raghavendra T. Cardiopulmonary efficiency in gutkha chewers: An Indian study. J Med Investig Pract [serial online] 2014 [cited 2018 Aug 24];9:74-8. Available from: http://www.jomip.org/text.asp?2014/9/2/74/139168 |
| Introduction | |  |
Mankind has used tobacco in various forms for 1000 years. Tobacco has been used orally alone or in combination with other ingredients. In India, tobacco is used in several forms such as pan (betel quid), dried leaves (Patti), paste (Kiwan, Zarda), tobacco with lime (Khaini/Mawa). [1] There has been resurgence of smokeless tobacco use since 1970, [2] its use is common in various parts of the world, including India and central Asia. An increase in consumption of smokeless tobacco has been noticed among high school, college students and sportspersons. [3],[4],[5] Use of smokeless tobacco indeed represents a health concern of growing magnitude among these groups. As a consequence of its addictive qualities, the consumption of smokeless tobacco often becomes a lifelong habit with cumulative and deleterious effects on health. [6],[7] Despite the known health consequences of tobacco, "chewing" is not viewed by users as particularly dangerous and is considered less of a "social evil" than smoking by much of the public. [8],[9] Smokeless tobacco has been advocated as a substitute for cigarette smoking. On the contrary, the use of smokeless tobacco is fraught with health risk and needs to be discouraged. Previous reports have described long term harmful effects of nicotine on various body parameters, little is known about acute effect of smokeless tobacco on cardiopulmonary parameters. [10] The effect of tobacco smoking on aerobic capacity and their predisposition to various unfavorable risk factors for disease is well-studied. There is paucity of studies indicating effect of use of gutkha, a common form of smokeless tobacco in India on cardiopulmonary parameters of youngsters.
Aims and objectives
This study has been undertaken to study the acute effect of gutkha chewing on cardiopulmonary efficiency tests in young healthy gutkha chewers when compared to age and sex matched nongutkha chewing healthy controls.
A sample size of 40 was taken in the study group and control each. This was a time bound study; hence this sample size was selected for statistical reasons.
This study was done in our physiology laboratory.
The subjects were selected from the general public on an outreach basis.
Informed consent was obtained from all participants.
| Materials and methods | |  |
This study was conducted in the Exercise Physiology Lab of PES IMSR, Kuppam, India. Forty apparently healthy sedentary male gutkha chewers of age group 18-25 years were taken as subjects and equal number of age and sex matched healthy nongutkha chewers were taken as controls. Ethical clearance was obtained from institution ethics committee.
The subjects for the study were selected based on the following criteria.
Inclusion criteria
- Males between 18 and 25 years of age
- Leading sedentary life
- Chewing gutkha for 4-5 years duration of five or more packets/day.
Exclusion criteria
- Age more than 25 years
- Leading physically active lifestyle
- Suffering from cardiopulmonary or systemic illness like diabetes, hypertension
- Involved in any sports or exercise regimen
- Addicted (dependence) to any drugs.
The subjects for the control group were selected based on the following criteria.
Inclusion criteria
- Males between 18 and 25 years of age
- Leading sedentary life
- Not chewed even a single packet of gutkha up to the time of study.
Exclusion criteria
- Age more than 25 years
- Leading physically active lifestyle
- Suffering from cardiopulmonary or systemic illness such as diabetes, hypertension
- Involved in any sports or exercise regimen
- Addicted (dependence) to any drugs.
Before starting the actual study subjects were briefed about the protocol and informed consent was obtained. Thorough history regarding suitability as per the above inclusion and exclusion criteria was elicited. Basic clinical examination was done to rule out any cardiopulmonary or other illness. Subjects were instructed to come to the lab and chew two packets of gutkha immediately before starting the recordings. Both controls and chewers were advised to refrain from consumption of coffee, tea and heavy meals at least 2 h prior to the recordings.
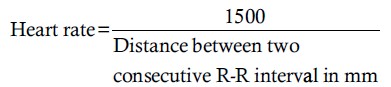
Resting heart rate
Resting heart rate (HR) was measured in both study and control group, with the help of Cardiart electrocardiograph (ECG) which is a single channel, 12 lead selection ECG, designed to record ECGs.
Measurement was carried out only after the subjects were thoroughly acquainted with working of the corresponding instrument and the prescribed maneuver.
Special instructions
- The subject was made to rest for 15 min after the attachment of leads
- He was instructed to remain in sitting posture and completely relaxed.
The calibration (1 mv = 10 mm deflection height) and paper speed (25 mm/s) were checked. Lead selection was switched to lead-II and ECG was taken. The resting HR was calculated and results were expressed as beats per minute.
Maximal voluntary ventilation
Maximal voluntary ventilation (MVV) was measured in both the study and the control group with the help of computerized spirolyser.
Recording of maximal voluntary ventilation
The sensor was placed on the stand and then MVV key was pressed. The subject was instructed to keep the disposable mouthpiece attached to pneumotachograph half way in the mouth above the tongue. The nose clip was applied and the start button was pressed. The subject was asked to breathe as deeply and as quickly as possible for 12 s, at the end of which the test terminates automatically. Now the sensor is replaced back on the stand. The screen displays the values of MVV along with its graph. This test has no memory. The print key was pressed to obtain a print.
Maximal oxygen consumption
Maximal oxygen consumption (VO 2 max) was indirectly assessed by the astrand-astrand nomogram method from submaximal exercise data obtained, while running on a treadmill.
Submaximal exercise testing
Subject preparation
- Subjects had to appear for the test only after 2-3 h have lapsed after the last meal
- Contra-indications to testing are ruled out
- A detailed explanation of the testing procedure was given outlining risks and possible complications. The subject was told how to perform the exercise test and the testing procedure was demonstrated
- All safety measures for the exercise testing were undertaken.
The treadmill was set to the elevation of 8°. The safety key was put in place and the mains switched ON. The subject was made to stand on the belt and support his arms by the side in the arm support provided. ECG limb leads were connected and the cables were securely tied to the legs. The ear pulse sensor was connected.
The "ON" switch is pressed to start the motor. The "FAST" switch is pressed to increase the speed gradually up to 5 km/h and the subject is instructed to run at this speed. The running is continued utnil a HR between 125 and 170 bpm is obtained as shown on the liquid-crystal display (LCD). A steady HR for a given work load is indicated by a variation of not more than 5 bpm. On attaining this HR, the speed is gradually brought down by pressing the slow switch and the machine is switched OFF.
Lead II is selected in the ECG machine and ECG is recorded for a few complexes and submaximal HR is calculated.
The distance travelled and time taken is noted down from the LCD display.
The power reached is calculated as follows:
X =sin�α ×B
Where,
- X = Vertical distance travelled
- α = Elevation in degrees
- B = Distance travelled on
- treadmill (in km)
- Work done = Weight of subject × (X)
- Power = Work done/time.
The Astrand nomogram is used. The HR and the power reached are connected in the nomogram. VO 2 max (in l/min) is read from the VO 2 scale.
Corresponding values of VO 2 max in terms of body weight, height, and surface area are calculated.
Since the subjects in this study did not exceed 25 years of age, age correction factor was not applied.
Maximal exercise testing
This is done after a rest period of 10 min. The LCD display of the treadmill is reset to 0 values.
The spirolyser is switched ON, subject's details entered and the volume-control (VC) key is pressed and kept ready. The ECG limb leads are connected and the cables secured as before. The subject was suitably instructed about the test maneuver. Elevation was continued at 7°. The subject was asked to run until exhaustion and to stop only when he felt that he could no longer run.
With the subject on the belt, the treadmill was switched ON and the FAST key pressed. The speed was gradually raised to 10 km/h. When the subject could no longer continue running, the speed was gradually brought down and the treadmill switched OFF.
Lead II is selected in the ECG machine and ECG is recorded for a few complexes and maximal HR is calculated.
Maximal heart rate
Simultaneously, the nose clip is applied; the disposable mouth piece on the pneumotachograph of the ready spirolyser is placed on the subject's mouth over the tongue. The start switch is pressed in the VC mode to record the respiration at VO 2 max work load. After 50 s the test terminates automatically. The sensor is placed back in its place. A print is obtained.
Delta heart rate
The delta HR was the calculated difference between the maximal HR and the resting HR.
Minute volume at maximal oxygen consumption
Minute volume at VO 2 max maximum minute ventilation (V E max) is calculated from the respiratory rate and the tidal volume recorded.
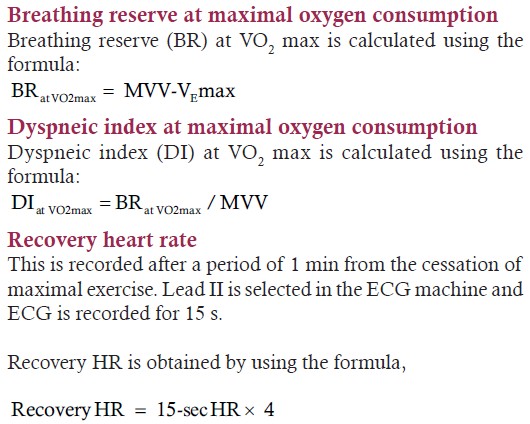
Maximum oxygen pulse
This is calculated by using the formula,

All these set of recordings were done on both the non-athlete as well as the athlete groups.
Statistical analysis was performed by using un-paired Student's test.
| Results | |  |
It is clear from [Table 1] that the controls and gutkha chewers were anthropometrically similar. From [Table 2], [Table 3], [Table 4], [Table 5] it is seen that gutkha chewers had a significantly higher resting heart rate whereas all other cardiopulmonary parameters showed no statistically significant difference.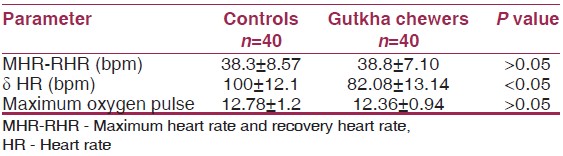 | Table 3: Comparison of the differences between (1) MHR-RHR, (2) maximum HR and resting HR (ä HR), (3) maximum oxygen pulse of controls and gutkha chewers
Click here to view |
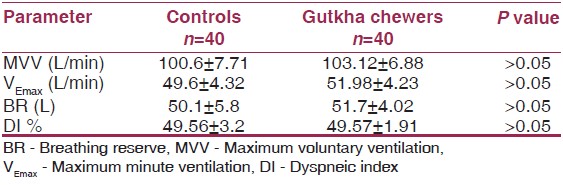 | Table 5: Comparison of the differences between (1) MVV, (2) VEmax, (3) DI of controls and gutkha chewers
Click here to view |
| Discussion | |  |
Previous workers have indicated acceleration or aggravation of cardiovascular disease as a result of tobacco in various forms. [11] In a study of the cardiovascular effects of daily smokeless tobacco use, the prominent effects of nicotine use viz., HR acceleration and increased urinary catecholamine excretion were similar throughout the day in people smoking cigarettes and those using smokeless tobacco. [10]
In this study, the resting HR was found to be statistically significantly higher in the study group. This is attributable to the lower vagal tone in gutkha chewers as a result of nicotine use even in the short term of 4-5 years which becomes apparent as an acute effect. This finding is in agreement with other studies. [12]
The delta HR was found to be statistically significantly lower among gutkha chewers. Delta HR is a long-term predictor of cardiovascular mortality independent of age, physical fitness and conventional coronary risk factors. [13] The lower delta HR suggests that gutkha chewers are at a higher risk for cardiovascular mortality.
There was no significant difference seen in parameters like VO 2 max, maximum oxygen pulse, MVV, V E max as an acute effect of gutkha chewing. Most of the workers had attributed decreased VO 2 max among smokers to the carbon monoxide saturation and less hemoglobin availability to carry oxygen. Our study group did not show any significant change in VO 2 max as carbon monoxide is nonexistent in smokeless tobacco.
In this study, it appears that tobacco chewers are physically fit like controls, but after immediate tobacco chewing a lesser delta HR suggests a higher risk for cardiovascular mortality.
Respiratory parameters show marginal increase in values. This could be due to bronchodilatation due to the release of epinephrine or stimulation of sympathetic system or both.
Stopping tobacco chewing at this juncture can be helpful HR, recovery HR, and delta HR can be used as prognostic assessment tools for any intervention therapy to stop gutkha chewing in asymptomatic individuals.
| References | |  |
| 1. | Health effects of smokeless tobacco. Council on scientific affairs. JAMA 1986;255:1038-44. 
|
| 2. | Gupta R, Gurm H, Bartholomew JR. Smokeless tobacco and cardiovascular risk. Arch Intern Med 2004;164:1845-9. 
|
| 3. | Sankaranarayanan R, Duffy SW, Padmakumary G, Day NE, Padmanabhan TK. Tobacco chewing, alcohol and nasal snuff in cancer of the gingiva in Kerala, India. Br J Cancer 1989;60:638-43. 
|
| 4. | Jones RB. Use of smokeless tobacco in the 1986 World Series. N Engl J Med 1987;316:952. 
|
| 5. | Hunter SM, Croft JB, Burke GL, Parker FC, Webber LS, Berenson GS. Longitudinal patterns of cigarette smoking and smokeless tobacco use in youth: The Bogalusa Heart Study. Am J Public Health 1986;76:193-5. 
|
| 6. | Schroeder KL, Chen MS Jr. Smokeless tobacco and blood pressure. N Engl J Med 1985;312:919. 
|
| 7. | Tomar SL, Giovino GA. Incidence and predictors of smokeless tobacco use among US youth. Am J Public Health 1998;88:20-6. 
|
| 8. | Rothman KJ. Tobacco habits. Am J Public Health 1986;76:133. 
|
| 9. | Marty PJ, McDermott RJ, Williams T. Patterns of smokeless tobacco use in a population of high school students. Am J Public Health 1986;76:190-2. 
|
| 10. | Siegel D, Benowitz N, Ernster VL, Grady DG, Hauck WW. Smokeless tobacco, cardiovascular risk factors, and nicotine and cotinine levels in professional baseball players. Am J Public Health 1992;82:417-21. 
|
| 11. | Benowitz NL. Systemic absorption and effects of nicotine from smokeless tobacco. Adv Dent Res 1997;11:336-41. 
|
| 12. | Bolinder GM, Ahlborg BO, Lindell JH. Use of smokeless tobacco: Blood pressure elevation and other health hazards found in a large-scale population survey. J Intern Med 1992;232:327-34. 
|
| 13. | Sandvik L, Erikssen J, Ellestad M, Erikssen G, Thaulow E, Mundal R, et al. Heart rate increase and maximal heart rate during exercise as predictors of cardiovascular mortality: A 16-year follow-up study of 1960 healthy men. Coron Artery Dis 1995;6:667-79. 
|
[Table 1], [Table 2], [Table 3], [Table 4], [Table 5]
|